What is Piriformis Syndrome, and do I have it?
Make it stand out
Piriformis Syndrome affects between 6 to 36 percent of low back pain patients.
What is the Piriformis muscle?
A stock image of a woman stretching on a floor mat.
The piriformis muscle is located in the buttocks near the hip joint and helps stabilize that joint when walking. The piriformis muscle connects the top of each femur to the base of the lumbar spine. It assists in rotating the hip and turning the leg and foot outward. The sciatic nerve passes under the piriformis muscle; a small percentage of the population may have the sciatic nerve running through the muscle. When a person has Piriformis Syndrome, they likely have chronic and intense pain mimicking sciatica since the muscle is compressing or irritating the sciatic nerve.
Since Piriformis Syndrome doesn't show up on scans, such as MRIs, CT scans, or X-rays, it's hard to diagnose. There is no definitive medical test that indicates Piriformis Syndrome. Since it is rare, many doctors don't recognize it when seeing Piriformis Syndrome in a patient. In March 2015, Drs. Hal David Martin, Manoj Reddy, and Juan Gomez-Hoyos proposed that Deep Gluteal Syndrome is a more appropriate term for the condition. The reasoning is that many structures, including the piriformis muscle, can cause sciatic nerve entrapment in the gluteal space.
How is Piriformis Syndrome Diagnosed?
Much of the diagnostic process for Piriformis Syndrome involves ruling out other potential causes of the pain, such as lumbar spine irregularities or injuries. The method depends on reviewing the patient's medical history, knowledge of spinal health and abnormalities, and patient reports of pain and other symptoms.
In Western medicine, treatment and diagnoses for any medical condition or disease are based on objective measures such as blood work, labs, and traditional diagnostic imaging and physical examinations.
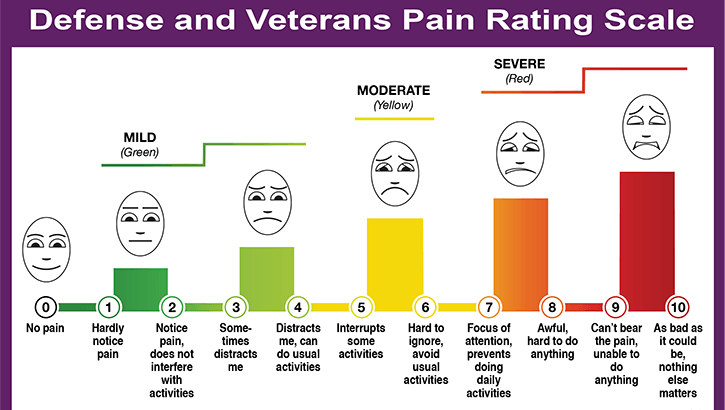
Pain, however, is subjective, and every patient experiences it differently. Therefore, pain treatment depends on medical personnel viewing the patient as a credible reporter of their pain.
This dynamic can put the patient at odds or in conflict with the caregivers charged with their treatment.
Many patients with Piriformis Syndrome benefit from nonoperative treatment such as physical therapy, anti-inflammatory medications, and local steroidal injections. However, there is a small subset of patients for whom nonoperative measures won't be successful, and the patient will require surgical decompression of the sciatic nerve. There are instances where a patient who receives surgical decompression develops scar tissue around the sciatic nerve; scar tissue can contribute to continued symptoms, and in such cases, the scar tissue may require surgery to remove.
My Personal Experience with Piriformis Syndrome and Lumbar Spine Pain
In 2017, I suffered from debilitating lower back, leg, and foot pain that I now know to be (in part) Piriformis Syndrome. In 7-1/2 months, I saw five physicians and specialists. I started with my general practitioner, was referred to three orthopedic surgical specialists, and then came a pain management specialist and an anesthesiologist. In the midst of it all, one emergency physician saw me for a total of nine minutes. (I was charged over $900 in copays for the privilege of those nine minutes.)
I was told repeatedly by these physicians that the symptoms I described and the pain levels I felt were "not justifiable." My MRI scans and X-rays showed moderate degenerative disc disease, four bulging/herniated discs in my lumbar spine, and osteoarthritis in my spinal column. Still, no one could see what was happening in my gluteus muscles.
Doctors told me time and again that I couldn't be experiencing the symptoms I was reporting. These symptoms included numbness in my left leg and chronic pain, reaching a ten on a 1-10 pain scale and staying there, 24/7, for years. I couldn't find any relief for the pain, not spinal injections or a myriad of medications, and I was in just as much pain lying down as I was sitting up or standing.
This is a great updated pain scale implemented by the US Department of Defense in recent years. I encourage patients to download it and share it with their doctors at future visits.
Finally, after nearly eight months, I was referred to a pain intervention specialist at a local hospital's neurology clinic, who listened and believed me. After a set of sacroiliac joint injections failed to provide relief, and in consideration of my health history and other symptoms such as numbness and tingling in my left leg and foot, I was diagnosed with Piriformis Syndrome.
After working with my pain interventionist for two months, we had a diagnosis that hadn't been reached in the previous months by five physicians and specialists. I believe the critical difference in treatment was my newest doctor trusted me to be an accurate reporter of my pain and symptoms where the others had not.
Piriformis Syndrome is in a pain class all its own.
In 2018, I had three sets of local steroidal injections into my piriformis muscle. These injections provided significant relief, allowing me to walk unassisted, drive myself to various appointments and treatment centers, and participate in water aerobics and muscle training sessions as part of my continued rehabilitation.
However, after 12 months, my pain specialist openly admitted to me in December of 2018 that he was just not sure what to do for me long-term. That's what it is like to have a rare medical condition; sometimes you have to make up or find your own answers, be your own case study. My physician and I had hoped that because I had such success with my first round of steroidal injections, physical therapy, and continued rehab would resolve my pain, at least mostly. However, the most extended period of relief I have experienced is about six weeks, the shortest just two or three weeks.
Due to high out-of-pocket costs and increased risk of infection and scar tissue, local injections were not a suitable long-term solution. Ultimately, in December of 2018, I received a dorsal column spinal cord stimulator implant that interrupts the pain signals that my brain receives from my left leg. The stimulator has, over time, re-trained my brain so that it doesn’t receive those pain signals as pain; instead, I feel a tingling sensation a lot like I am wearing a TENS unit (affiliate link.) My daily baseline pain in my left leg is now about two or three on a 1-10 pain scale, and rarely does the pain break through and flare drastically these days, though it does like to make sure to be remembered from time to time. a literal cyborg! Neat, eh? Stay tuned for a blog on what it’s like to get that implant.
Living with Piriformis Syndrome
I encourage anyone with chronic pain symptoms such as I have described here to explore the possibility of a Piriformis Syndrome or Deep Gluteal Syndrome diagnosis with your physician. If you find that your doctor(s) won't listen to you, know you are not alone, especially if you are a woman.
In the years since my original diagnosis, I've been diagnosed with several chronic pain conditions and diagnoses related to my spine. Piriformis Syndrome wasn't the only thing I had brewing in my body. Still, it certainly had some of the most immense impact on my quality of life.
Kelly J. Mendenhall is smiling and posing in front of a turquoise-colored wall, wearing a purple dress adorned with cartoon dinosaurs.
In a study observing gender-related pain biases, researchers found that there was a "growing body of evidence" that indicated significant differences in pain response and treatment between men and women. Women are more likely to experience pain and be more sensitive to it. When it comes to pain as sharp as piriformis syndrome, it's no wonder women notice it more often than men. Robert H. Shmerling, MD, associate professor of medicine at Harvard Medical School and Clinical Chief of Rheumatology at Beth Israel Deaconess Medical Center in Boston, says Piriformis Syndrome appears more prevalent among women. However, the reason for this has yet to be discovered.
Other risk factors of Piriformis Syndrome include, but are not limited to:
being overweight/obese,
a history of sciatic nerve pain, bulging discs, anatomical abnormality in the piriformis muscle, or
other spinal problems.
The procedures and lifestyle changes I've implemented in the years since being diagnosed with Piriformis Syndrome have all significantly decreased my daily pain. Don’t shoot the messenger; they include:
An anti-inflammatory diet (loose, I'm not fanatic or obsessive about it anymore)
daily stretches, targeted muscle movements and exercises, and
a dorsal column spinal cord stimulator implant.
We, as patients, are our own best advocates. If you feel that your physician is not treating you well or not hearing you regarding your pain and other symptoms, request a referral to another physician; do it again and again until you find the right one. Medical gaslighting is killing and disabling women daily, and it’s beyond time to stop it.
We all deserve the best quality of life afforded to us, and just because we don't fit into any particular medical checkbox doesn't mean we aren't experiencing real symptoms and legitimately debilitating pain.
Disclaimer:
Information provided within this article is for educational purposes and is not a substitute for medical advice. Those seeking specific medical advice should consult their doctor or surgeon.
Note:
Kelly J. Mendenhall originally wrote this article as a guest author for SpineNation in 2019. (SpineNation closed its doors in the Fall of 2021.) A blog entry for Nerdzilla Lives! inspired the content, which was updated and rewritten in August 2024.